The Complete Guide for Professionals, Researchers, and Entrepreneurs
Introduction
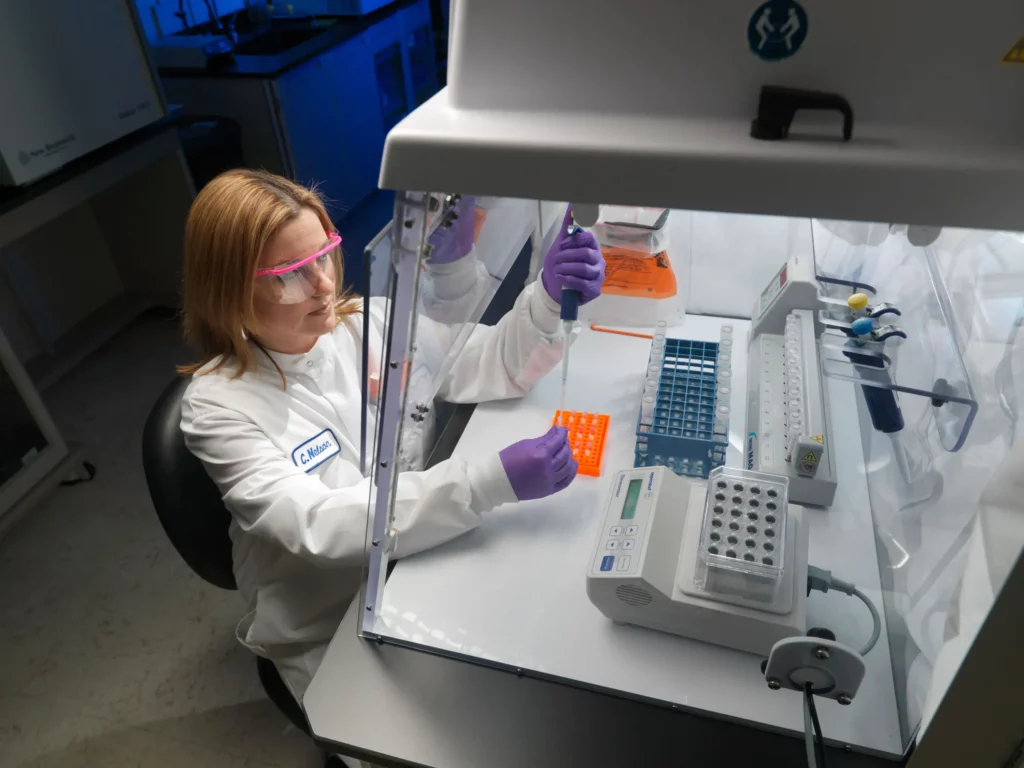
A clinical research laboratory is a center of innovation, discovery and quality control in the field of healthcare, biotechnology, pharmaceuticals, and education. To professionals, researchers as well as business owners, the creation of a clinical research lab is a sound investment that requires careful planning, regulation, and a clear grasp of technology and market requirements. This manual addresses all the elements of establishing a clinical research laboratory, infrastructure, equipment, workflow, staffing, safety and business strategy. All through, key words like establishment of clinical research laboratories, equipment of clinical research laboratories, business plan of a laboratory and laboratory accreditation are used as friendly keywords that are incorporated to ensure maximum search visibility.

What is a Clinical Research Lab?
A clinical research laboratory refers to a special laboratory where biological samples (blood, tissue, urine, among other fluids) are tested to provide support to clinical trials, medical research, diagnostics, and product development. These labs are vital in hospitals, research institutes, pharmaceutical firms, contract research organizations (CRO) and in learning institutions.
Key Functions of a Clinical Research Laboratory
- Clinical Trials Support: Processing and analysis of drug and device study samples.
- Biomarker Discovery: The discovery and validation of new disease biomarkers.
- Diagnostics Development: Creating and validating new diagnostic tests.
- Pharmacokinetics and Pharmacodynamics: Studying drug absorption, distribution, metabolism, and excretion.
- Quality Control: Making sure that there is integrity of data and adherence to regulations.
- Education and Training: Providing hands-on experience for students and professionals.
Planning Your Clinical Research Lab
1. Define Your Lab’s Purpose
- Medical Research: Clinical trials, biomarker research and translational research.
- Pharmaceutical/Industrial: Assistance in the development of drugs, toxicology, and testing of the product.
- Educational: Provide the training of research methods and laboratory procedures.
2. Market Analysis and Business Plan
- Target Market: Hospitals, pharma/biotech companies, academic institutions, CROs.
- Competitive Analysis: Evaluate local competitors and regional competitors, their services and prices.
- Regulatory Landscape: Understand licensing, accreditation, and compliance requirements (e.g., NABL, CAP, CLIA, ISO 15189).
- Financial Projections: Estimate startup costs, operational expenses, and revenue streams.
- Business Model: Define your service offerings, pricing strategy, and value proposition.
3. Facility and Infrastructure
- Location: Select an easy-access site where clients and samples can be picked.
- Space Planning: Designate space to receive samples, process them, analyze, store and disposal.
- Utilities: Ensure reliable water supply, drainage, electricity (with backup), and ventilation.
- Sanitation: Use materials for walls, ceilings, and floors that are easy to clean and resistant to biohazards.
- Security: Restrict access to authorized personnel only.
Essential Equipment and Instruments
A well-equipped clinical research lab should have the following core instruments.
| Equipment | Purpose/Function |
|---|---|
| PCR Machine (Thermal Cycler) | Amplifies DNA/RNA for analysis |
| Centrifuge | Separates components based on density |
| Gel Electrophoresis System | Separates DNA, RNA, or proteins |
| Spectrophotometer | Quantifies nucleic acids and proteins |
| Microplate Reader | Measures absorbance, fluorescence, or luminescence |
| Biosafety Cabinet | Protects samples and personnel from contamination |
| Laminar Air Flow Hood | Provides aseptic workspace |
| Incubator | Maintains optimal temperature for cultures/reactions |
| Deep Freezer (-80°C) | Stores reagents and biological samples |
| Refrigerated Centrifuge | Processes temperature-sensitive samples |
| Analytical Balance | Precise weighing of samples and reagents |
| Micro Pipettes | Accurate liquid handling |
| Water Bath | Maintains constant temperature for reactions |
| Vortex Mixer | Mixes solutions quickly and efficiently |
| Computer & Printer | Data management and reporting |
| Ultra-Low Temperature Freezer | Long-term storage of sensitive samples |
| ELISA Reader | Quantifies antigen-antibody reactions |
| Automated Liquid Handler | High-throughput sample processing |
| Fume Hood | Safe handling of volatile chemicals |
| Cryostat | Sectioning of frozen samples |
| Flow Cytometer | Cell analysis and sorting |
Tailor this list to your lab’s specific focus (clinical, research, industrial, or educational).
Laboratory Design and Workflow
Layout Considerations
- Reception and Accessioning Area: For sample registration and drop-off.
- Sample Processing Room: For centrifugation, aliquoting, and preparation.
- Analytical Section: Houses major instruments and testing stations.
- Molecular Biology Area: For PCR, sequencing, and genetic analysis.
- Data Analysis and Reporting: Secure space for bioinformatics and result interpretation.
- Storage: For samples, reagents, and hazardous materials.
- Waste Management: For safe disposal of biohazardous and chemical waste.
- Administrative Office: For documentation, billing, and communication.
Workflow Optimization
- Unidirectional Flow: Ensure samples move in one direction to minimize cross-contamination.
- Zoning: Separate clean and contaminated areas.
- Automation: Implement Laboratory Information Management Systems (LIMS) for tracking and reporting.
- Open-Plan Designs: Enable flexible reconfiguration and lean operations.
- Contingency Planning: Prepare for equipment failure, power outages, and emergencies.
Staffing and Training
Key Personnel
- Lab Director/Manager: Oversees operations, compliance, and quality assurance.
- Principal Investigators/Scientists: Lead research projects and protocol development.
- Medical Laboratory Technologists: Perform routine and specialized analyses.
- Research Associates/Assistants: Support experiments and data collection.
- Bioinformaticians: Analyze sequencing and omics data.
- Technical Assistants: Maintain equipment and manage supplies.
- Administrative Staff: Handle billing, logistics, and customer service.
Training and Competency
- Initial Training: On SOPs, equipment use, and safety protocols.
- Ongoing Education: Updates on new technologies, quality standards, and regulatory changes.
- Competency Assessment: Regular evaluation to ensure proficiency and compliance.
Safety and Quality Assurance
Safety Measures
- Personal Protective Equipment (PPE): Lab coats, gloves, eye protection, and masks.
- Biosafety Cabinets: For handling infectious materials.
- Chemical Safety: Proper storage, labeling, and handling of reagents.
- Fire Safety: Extinguishers, alarms, and emergency exits.
- Waste Disposal: Segregation and safe disposal of biological and chemical waste.
- Biosafety Level 2/3 (BSL-2/3): For handling infectious disease samples, with specialized ventilation and access controls.
- Emergency Procedures: Clear protocols for spills, exposures, and accidents.
Quality Control
- Internal QC: Regular calibration of instruments, use of control samples.
- External QC: Participation in proficiency testing programs.
- Documentation: Maintain detailed records of procedures, results, and incidents.
- Accreditation: Seek certification from recognized bodies (e.g., NABL, CAP, ISO 15189).
Common Clinical Research Lab Services
| Service Type | Description | Clinical/Research Relevance |
|---|---|---|
| Sample Processing | Blood, tissue, urine, and other fluids | Clinical trials, diagnostics, biobanking |
| Molecular Diagnostics | PCR, qPCR, sequencing, genotyping | Infectious diseases, oncology, genetics |
| Biomarker Analysis | ELISA, immunoassays, mass spectrometry | Drug development, disease monitoring |
| Cell Culture | Primary cells, immortalized lines | Drug screening, toxicity studies |
| Flow Cytometry | Cell population analysis and sorting | Immunology, hematology, cancer research |
| Biochemical Analysis | Enzyme activity, metabolite quantification | Metabolic disorders, pharmacology |
| Imaging and Microscopy | Light, fluorescence, confocal microscopy | Cell biology, pathology, morphometrics |
| Data Management | LIMS, statistical analysis, bioinformatics | Regulatory compliance, research integrity |
Regulatory Compliance and Accreditation
- Licensing: Obtain necessary licenses from local and national authorities (e.g., NABL in India, CLIA, ISO 15189).
- Accreditation: Demonstrates adherence to international quality standards.
- Quality Management System: Implement SOPs, equipment logs, and personnel records.
- Audit Readiness: Regular internal and external audits to ensure compliance.
- Data Security: Ensure patient and research data are securely stored and privacy is maintained.
Budgeting and Financial Planning
Startup Costs
- Infrastructure: Renovation, utilities, and security.
- Equipment: Purchase, installation, and calibration.
- Consumables: Reagents, glassware, PPE, and disposables.
- Staffing: Salaries, training, and benefits.
- Licensing and Accreditation: Application fees and inspection costs.
Operational Expenses
- Reagent and Consumable Replenishment
- Equipment Maintenance and Service Contracts
- Utilities (Electricity, Water, Internet)
- Waste Disposal Services
- Insurance (Liability, Fire, Theft)
Revenue Streams
- Clinical Trial Services
- Research Contracts and Grants
- Diagnostic Testing
- Training and Educational Programs
- Consulting and Quality Assurance Services
Develop a detailed business plan with financial projections to attract investors and manage growth.
Marketing and Growth Strategies
- Digital Marketing: optimized website, social media, and online advertising.
- Partnerships: Collaborate with hospitals, clinics, CROs, and research organizations.
- Quality Differentiation: Emphasize accreditation, turnaround time, and advanced technology.
- Customer Service: Reliable reporting, transparent billing, and responsive support.
- Continuous Improvement: Invest in staff training, equipment upgrades, and new test offerings.
Trends and Innovations in Clinical Research Labs
- Automation and Robotics: Increase throughput, reduce errors, and improve reproducibility.
- Next-Generation Sequencing (NGS): High-throughput DNA/RNA sequencing for comprehensive analysis.
- Digital Pathology and Imaging: Integration of digital imaging and remote diagnostics.
- Artificial Intelligence: Advanced data analysis, pattern recognition, and predictive diagnostics.
- Point-of-Care Testing: Decentralized, rapid testing for clinical trials and field studies.
- Sustainable Practices: Green chemistry, energy-efficient equipment, and waste reduction.
Checklist for Setting Up a Clinical Research Lab
- Define lab purpose and scope
- Conduct market and competitor analysis
- Prepare a detailed business plan
- Secure funding and location
- Design lab layout and workflow
- Procure essential equipment and consumables
- Recruit and train qualified staff
- Implement safety and quality protocols
- Obtain necessary licenses and accreditations
- Launch marketing and outreach initiatives
Conclusion
Establishing a clinical research laboratory is a complex but rewarding endeavor that blends science, business, and regulatory compliance. By following best practices in planning, infrastructure, equipment selection, staffing, safety, and quality assurance, you can build a lab that meets the needs of healthcare, research, industry, or education. Stay updated with technological advancements and regulatory changes to ensure your lab remains competitive and compliant.
Keywords Used
- clinical research lab setup
- clinical research lab equipment
- clinical research laboratory business plan
- laboratory accreditation
- laboratory safety protocols
- clinical research tests
- laboratory workflow
- laboratory quality control
- clinical diagnostics
- research laboratory
- laboratory automation
- laboratory compliance
- laboratory marketing strategies